Pathophysiology of PAH
Pathophysiology of PAH

How does Pulmonary Arterial Hypertension (PAH) develop?
The exact causes behind the development of pulmonary arterial hypertension (PAH) remain unknown. However, research has led to a better understanding of the underlying pathological mechanisms.
What is PAH?
©Janssen-Cilag NV - EM-38436 - 21-jul-2020 - vu/er Luc Van Oevelen, Antwerpseweg 15-17, 2340 Beerse, ©Janssen-Cilag B.V. - EM-38436 - 21-jul-2020
The 2015 European Society of Cardiology and European Respiratory Society (ESC/ERS) guidelines classify pulmonary hypertension (PH) into five main groups, according to their similar clinical presentation, pathological findings, haemodynamic characteristics and treatment strategy.[1]
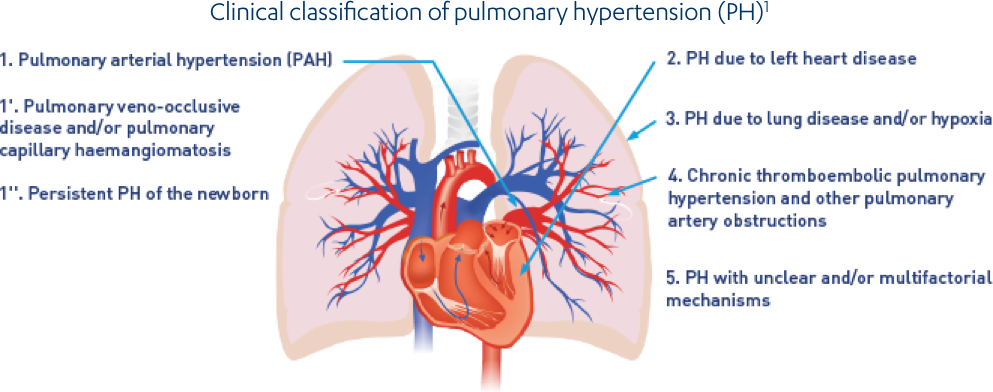
Adapted from Galiè et al. 2016[1]
These 5 PH groups are further subcategorised. [1]
1. PAH
1.1 Idiopathic
1.2 Heritable
1.2.1 Bone morphogenetic protein receptor type 2 (BMPR2) mutation
1.2.2 Other mutations
1.3 Drug- and toxin-induced
1.4 Associated with:
1.4.1 Connective tissue disease
1.4.2 Human immunodeficiency virus (HIV) infection
1.4.3 Portal hypertension
1.4.4 Congenital heart disease
1.4.5 Schistosomiasis
1'. Pulmonary veno-occlusive disease and/or pulmonary capillary haemangiomatosis
1’.1 Idiopathic
1’.2 Heritable
1’.2.1 Eukaryotic translation initiation factor 2 alpha kinase 4 (EIF2AK4) mutation
1’.2.2 Other mutations
1’.3 Drug-, toxin- and radiation-induced
1’.4 Associated with:
1’.4.1 Connective tissue disease
1’.4.2 HIV infection
1”. Persistent pulmonary hypertension of the newborn
2. PH due to left heart disease
2.1 Left ventricular systolic dysfunction
2.2 Left ventricular diastolic dysfunction
2.3 Valvular disease
2.4 Congenital/acquired left heart inflow/outflow tract obstruction and congenital cardiomyopathies
2.5 Congenital/acquired pulmonary veins stenosis
3. Pulmonary hypertension due to lung diseases and/or hypoxia
3.1 Chronic obstructive pulmonary disease
3.2 Interstitial lung disease
3.3 Other pulmonary diseases with mixed restrictive and obstructive pattern
3.4 Sleep-disordered breathing
3.5 Alveolar hypoventilation disorders
3.6 Chronic exposure to high altitude
3.7 Developmental lung diseases
4. Chronic thromboembolic pulmonary hypertension and other pulmonary artery obstructions
4.1 Chronic thromboembolic pulmonary hypertension
4.2 Other pulmonary artery obstructions
4.2.1 Angiosarcoma
4.2.2 Other intravascular tumours
4.2.3 Arteritis
4.2.4 Congenital pulmonary arteries stenoses
4.2.5 Parasites (hydatidosis)
5. Pulmonary hypertension with unclear and/or multifactorial mechanisms
5.1 Haematological disorders: chronic haemolytic anaemia, myeloproliferative disorders, splenectomy
5.2 Systemic disorders: sarcoidosis, pulmonary histiocytosis, lymphangioleiomyomatosis, neurofibromatosis
5.3 Metabolic disorders: glycogen storage disease, Gaucher disease, thyroid disorders
5.4 Others: pulmonary tumoural thrombotic microangiopathy, fibrosing mediastinitis, chronic renal failure (with/without dialysis), segmental pulmonary hypertension
PAH is subcategorised according to underlying disease pathogenesis.[1]
1.1 Idiopathic PAH (IPAH)
Accounting for 30–50% of cases, [2] IPAH is the most common form of PAH and describes sporadic disease in which both family history and identifiable risk factors are absent.[1]
1.2 Heritable PAH (HPAH)
HPAH accounts for ∼6% of PAH cases, and includes patients with a family history of the disease and those carrying a mutation in a gene known to be associated with PAH. Heterozygous mutations in the gene encoding the bone morphogenetic protein receptor type 2 (BMPR2) are the most common genetic defects seen.[3]
1.3 Drug- and toxin-induced PAH
PAH can be associated with exposure to certain drugs or toxins, particularly appetite suppressant intake drugs, such as aminorex, fenfluramine derivatives and benfluorex. These drugs have been confirmed to be risk factors for PAH and many have since been withdrawn from the market.[4]
1.4 Associated PAH
Approximately half of patients with PAH have an associated disease such as connective tissue disease, congenital heart disease, portal hypertension, HIV infection or schistosomiasis.[5]
Connective tissue disease (CTD-PAH)
CTD-PAH is the second most common subtype of PAH after IPAH, comprising up to 30% of cases.[2] PAH is most commonly seen in systemic sclerosis (SSc), accounting for almost 75% of CTD-PAH cases.[6] Approximately 1 in 10 patients with SSc are estimated to develop PAH.[7] The remaining cases of CTD-PAH are due to systemic lupus erythematosus (SLE, 8–19%), mixed connective tissue disease (MCTD, 8–9%), rheumatoid arthritis (RA, 3–5%), dermatomyositis/polymyositis (DM/PM, 4%), undifferentiated connective tissue disease (2%) and Sjögren's syndrome (1%).[6]
Congenital heart disease (CHD-PAH)
Accounting for 10–23% of PAH cases, CHD-PAH is the third most common PAH subtype[2] and represents a very heterogeneous patient population. The 2015 European Society of Cardiology and European Respiratory Society (ESC/ERS) guidelines provide a clinical classification of CHD-PAH:[1]
- Eisenmenger’s syndrome
- PAH associated with prevalent systemic-to-pulmonary shunts
- PAH with small/coincidental defects
- PAH after defect correction
Portal hypertension (PoPH)
Approximately 5–10% of patients with portal hypertension develop PAH.[2] Portopulmonary hypertension (PoPH) is associated with the presence of portal hypertension, not necessarily with the presence of liver disease. However, as cirrhotic liver disease is the most common cause of portal hypertension, PoPH is most frequently encountered in patients with cirrhosis.[1]
Human immunodeficiency virus (HIV-PAH)
PAH is a rare complication of HIV infection. It is likely that the modern management of HIV using highly active antiretroviral therapy has resulted in improved survival and decreased incidence of HIV-PAH. These effects on survival and incidence have resulted in a stable HIV-PAH prevalence of 0.5%.[1]
Schistosomiasis
In Brazil, where schistosomiasis infection is endemic, schistosomiasis-associated PAH is the third most common subtype, after IPAH and CTD-PAH, accounting for 20% of all cases.[2]
1’. Pulmonary veno-occlusive disease (PVOD) and/or pulmonary capillary haemangiomatosis (PCH)
PVOD/PCH is a difficult disorder to categorise, as it shares characteristics with IPAH but also has a number of distinct differences. The 2015 ESC/ERS guidelines classify PVOD/PCH as a distinct category but not completely separated from PAH.[1] The true incidence of PVOD/PCH is unknown because many cases are still misclassified as PAH; the proportion of IPAH cases that in reality fulfil the criteria for PVOD/PCH is likely to be around 10%.[1]
1’’. Persistent PH of the newborn (PPHN)
PPHN includes a heterogeneous group of conditions that may differ from classical PAH and, as a consequence, it has been subcategorised as group 1”.[1] It is a frequent cause of hypoxemic respiratory failure in term and late preterm infants affecting 0.43–6.8 per 1,000 live births.[8]
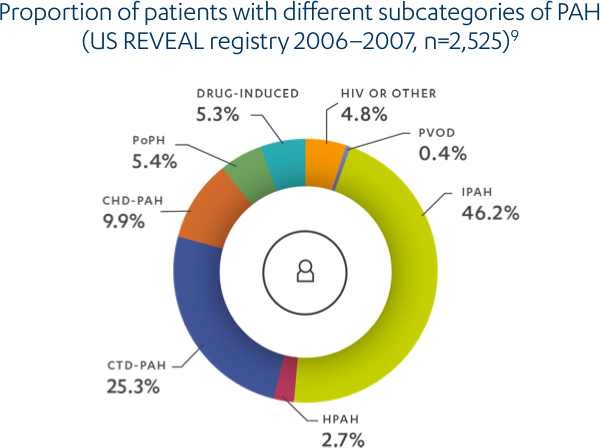
Adapted from Badesch et al. 2010 [9]
CHD, congenital heart disease; CTD, connective tissue disease; IPAH, idiopathic pulmonary arterial hypertension; HIV, human immunodeficiency virus; HPAH, heritable pulmonary arterial hypertension; PAH, pulmonary arterial hypertension; PoPH, portopulmonary hypertension; PVOD, pulmonary veno-occlusive disease.
PAH is a rare, progressive disease.[10] Without treatment, PAH carries a poor prognosis.[11] The course of PAH is variable and the rate at which disease progression occurs depends on the type of PAH as well as several other factors, such as the underlying aetiology of the patient's disease, age, associated conditions and comorbidities.[1],[12] While there is currently no cure for the disease, modern PAH therapies can markedly improve a patient's symptoms and slow the rate of clinical deterioration.[13]
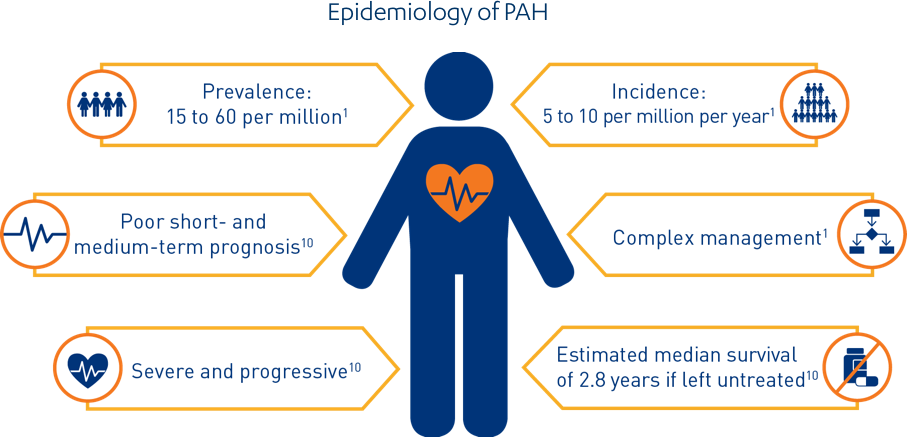
PAH, pulmonary arterial hypertension
Who is at risk?
A number of registries over the years have reported baseline characteristics and outcome data on >10,000 patients with PAH, providing important insights into the evolving epidemiology of PAH and facilitating the development of prognostic indicators for the disease.[2]
PAH aetiology
- PAH associated with congenital heart disease (CHD-HA)[1]
- PAH associated with systemic sclerosis (SSc-PAH)
SSc patients are at high risk of developing PAH,[14] which can be severe and fatal, and accounts for >50 deaths in these patients.[15] - PAH associated with portopulmonary hypertension (PoPH-PAH)
Patients with PoPH-PAH have also been identified as a higher risk cohort compared with IPAH.[16]
Age and sex
In general, registry data indicate a greater incidence of PAH in female patients; on average registries report 70–80% female patients with PAH. In the US registries, the proportion of female to male patients appears to have increased over time, with female patients accounting for 63% of IPAH patients in the NIH registry and 80% in the more recent REVEAL registry.[17]
While the mean age of patients with IPAH in the first US National Institutes of Health (NIH) registry created in 1981 was 36 years, PAH is now more frequently diagnosed in elderly patients, resulting in a mean age at diagnosis between 50 and 65 years in contemporary registries.[1]
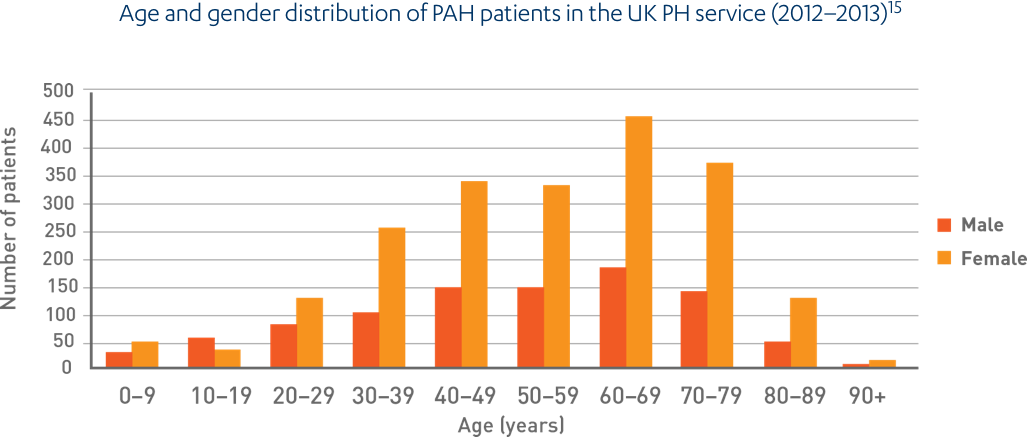
Adapted from National Audit of Pulmonary Hypertension 2013[18]
PAH, pulmonary arterial hypertension; PH, pulmonary hypertension
The increase in pulmonary vascular resistance (PVR) is related to different mechanisms and therefore PAH is recognised as a complex, multifactorial condition involving numerous biochemical pathways and different cell types.[19] Endothelial dysfunction is believed to occur early in disease pathogenesis, leading to endothelial and smooth muscle cell proliferation followed by structural changes or remodelling of the pulmonary vascular bed.[20],[19] The increase in pulmonary arterial pressure (afterload) makes the right heart work harder. Initially, the heart is able to compensate for the increased pressure; however, as the disease progresses, the right ventricle becomes dilated, eventually resulting in right ventricular failure and death.[19],[21]
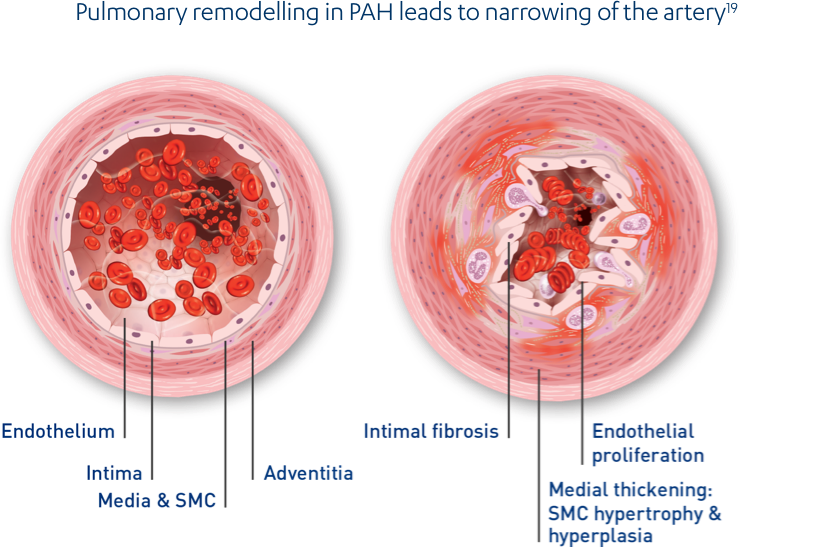
Adapted from Galiè et al. 2010[19]
PAH, pulmonary arterial hypertension; SMC, smooth muscle cell
Vascular remodelling
Every vessel wall layer is affected and multiple cell types are involved:[20],[19]
- Endothelial cells
- Smooth muscle cells
- Fibroblasts
- Inflammatory cells and platelets[19]
This endothelial dysfunction significantly impairs the production of vasoactive mediators such as nitric oxide and prostaglandin, while leading to the overexpression of vasoconstrictors such as endothelin-1 (ET-1),[20] ultimately leading to an increase in PVR.[19]
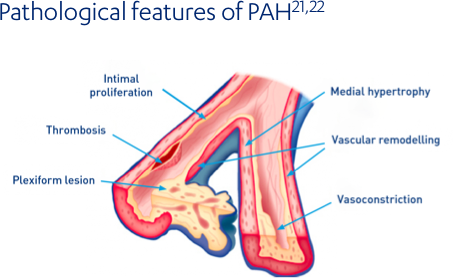
The prominent pathological features of PAH include:[22]
- Hypertrophy (increase in size) of cellular layers that line the blood vessels
- Development of plexiform lesions at arterial branch points
Adapted from Gaine et al. 2000[23]
PAH, pulmonary arterial hypertension
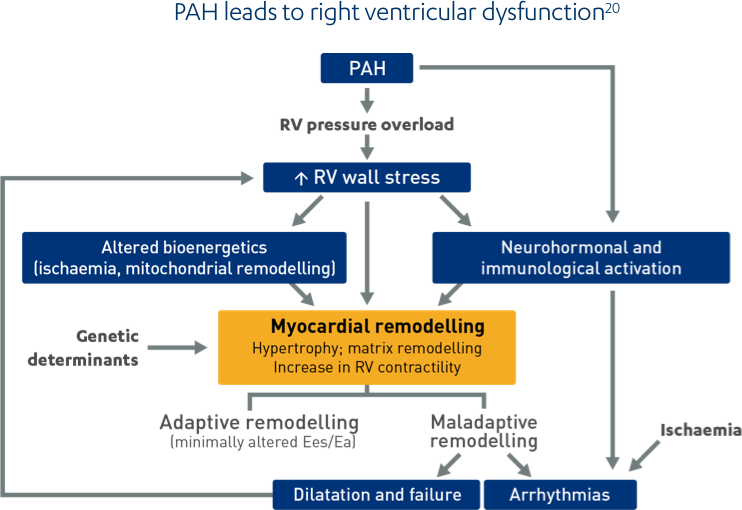
Adapted from Vonk Noordegraaf et al. 2013[21]
Ea, arterial elastance; Ees, end-systolic elastance; PAH, pulmonary arterial hypertension; RV, right ventricle
PAH affects the small vessels of the pulmonary circulation. Changes to the pulmonary vasculature lead to the typical symptoms of PAH. Symptoms, such as dyspnoea, are often non-specific and can be associated with a number of underlying conditions.[24]
These symptoms may be accompanied with a cough, sometimes with haemoptysis. Some patients may even develop hoarseness, caused by compression of a nerve in the chest by an enlarged pulmonary artery.[1] As PAH advances, patients can develop a bluish discolouration due to cyanosis. The continued strain on the heart can lead to swelling of the face, ankles, abdomen and feet due to oedema.[1] Too often patients only present when they are no longer able to continue with daily activities. By this time, the disease may have progressed to a point where the patient is bedridden from shortness of breath or other symptoms.
PAH, pulmonary arterial hypertension
You may also be interested in
Clinical guidelines set out the diagnostic pathway so patients can be referred and treated as quickly as possible.
Modern treatments can significantly improve patients’ symptoms and slow the rate of clinical deterioration.
Do you have a question for us or did you not find what you were looking for? Let us know and one of our Janssen-specialists will contact you as soon as possible.
Discover Janssen's portfolio and the matching SmPC's.
On this page you will find interactive 3D animations of the human anatomy and various syndromes. This allows you to zoom in on the anatomy, tissue structures, disease mechanisms and the course of the disease.